Clinical Background
Macular edema is a swelling of the central retina caused by excess fluid and indicates compromised function in blood-retinal barrier (Figure 1). It often occurs as a result of a retinal disease such as neovascular age-related macular degeneration (AMD), retinal vein occlusion (RVO) or diabetic macular edema (DME), and causes sudden and severe loss of vision, affecting a large number or people. Therapies with anti-vascular endothelial growth factor (Anti-VEGF) agents are highly effective and have revolutionized the treatment of macular edema. However the effectiveness of anti-VEGF drugs depends on frequent monitoring, early detection of reactivation of the disease and the extent of the present fluid.
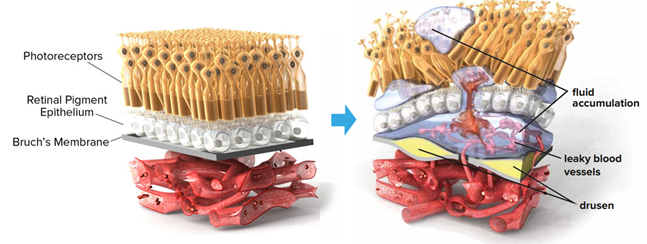
Figure1. Fluid leakage affecting the retina as a result of neovascularization in age-related macular degeneration (AMD). Courtesy of The Angiogenesis Foundation.
Retinal pathologies such as accumulated fluid can be imaged using spectral domain optical coherence tomography (SD-OCT), which is the most important ancillary test for the diagnosis of sight degrading diseases today. OCT is a non-invasive modality for acquiring high resolution, 3D cross sectional volumetric images of the retina and the sub-retinal layers, in addition to retinal pathology. OCT acquires a series of 2D slices (B-scans).
Three Fluid Types
Three types of fluid (Figure 2) are clinically distinguishable on OCT images and are part of this Challenge:
-
Intraretinal fluid (IRF) consists of contiguous fluid-filled spaces containing columns of tissue. These spaces may appear as separated hyporeflective cystoid pockets when viewed by OCT hence sometimes it is also referred to as intraretinal cystoid fluid.
-
Subretinal fluid (SRF) corresponds to the accumulation of a clear or lipid-rich exudate in the subretinal space, i.e., between the neurosensory retina and the underlying retinal pigment epithelium (RPE).
- Pigment Epithelial Detachment (PED) is specific to AMD and represents detachment of the retinal pigment epithelium (RPE, bright band at the bottom of the retina) along with the overlying retina from the remaining Bruch’s membrane by the accumulation of fluid. It appears as three subtypes: serous, fibrovascular or drusenoid. All three subtypes are considered and annotated as PED within the Challenge.
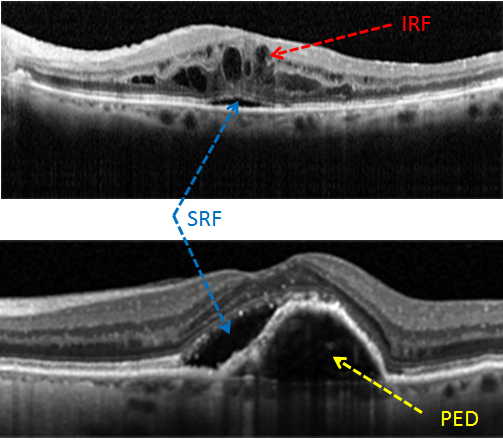
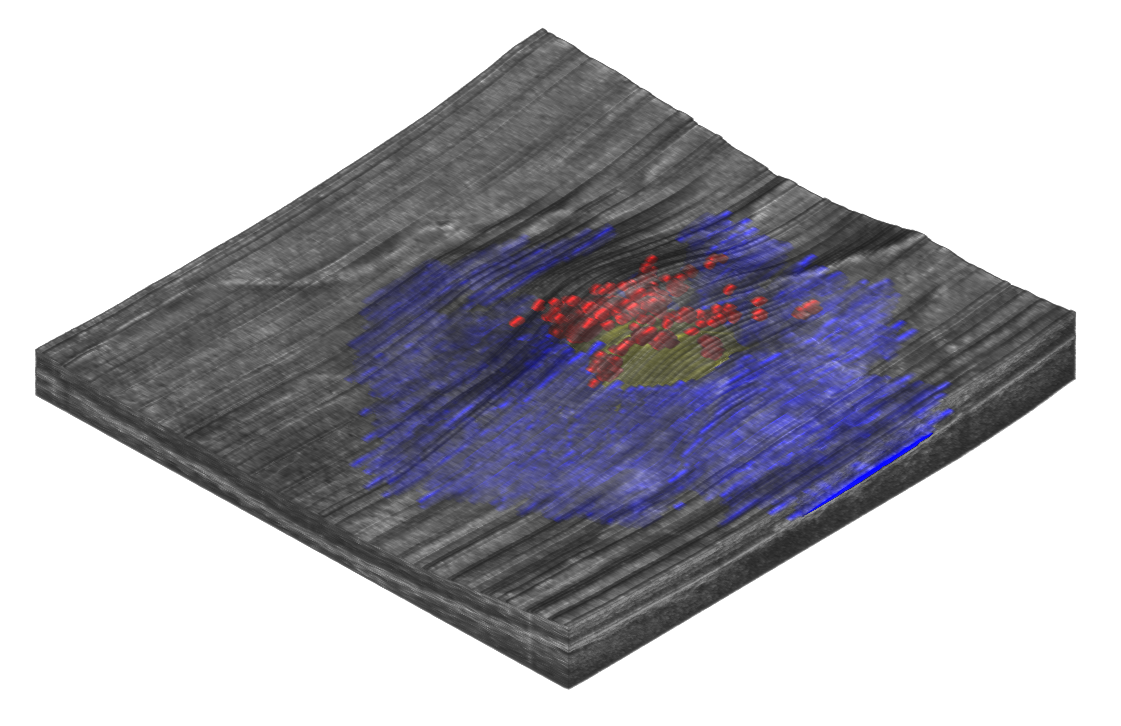
Figure 2. The three fluid types on an OCT slice (B-scan): Intraretinal Fluid (IRF) in red, Subretinal Fluid (SRF) in blue, and Pigment Epithelium Detachment (PED) in yellow. Volume rendering of different fluid inside the retina. All three subfigures come from three different patients
OCT Device Manufacturers
OCT images (Figure 3) are prone to motion artifacts between slices (B-scans) and low signal-to-noise ratio (SNR) due to speckle. There is a trade-off between SNR and spatial resolution thus some manufacturers acquire multiple B-scans at the same anatomical location to reduce noise on the expense of producing fewer B-scans.
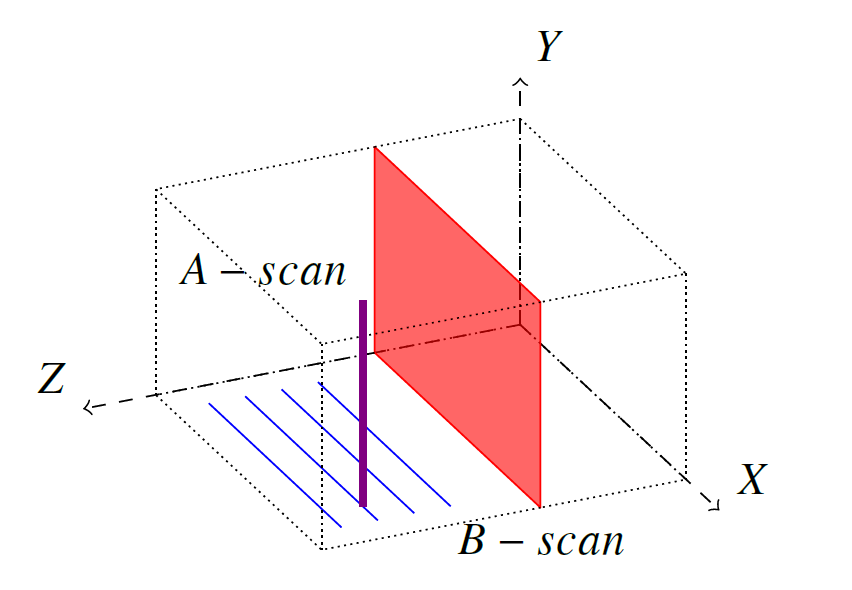
Figure 3. OCT acquisition and the coordinate system. 1D axial scans (A-scan, purple) are combined to form a 2D cross sectional slice (B-scan, red) by scanning through the volume in a raster scan pattern (blue). Multiple B-scans are then combined to form a complete OCT volume.
The images available in this Challenge are acquired with spectral-domain OCT imaging devices from three distinct manufacturers:
- Cirrus (Zeiss Meditec) with 128 B-scans.
- Spectralis (Heidelberg Engineering) with 49 B-scans.
- T-1000 and T-2000 (Topcon) with 128 B-scans.
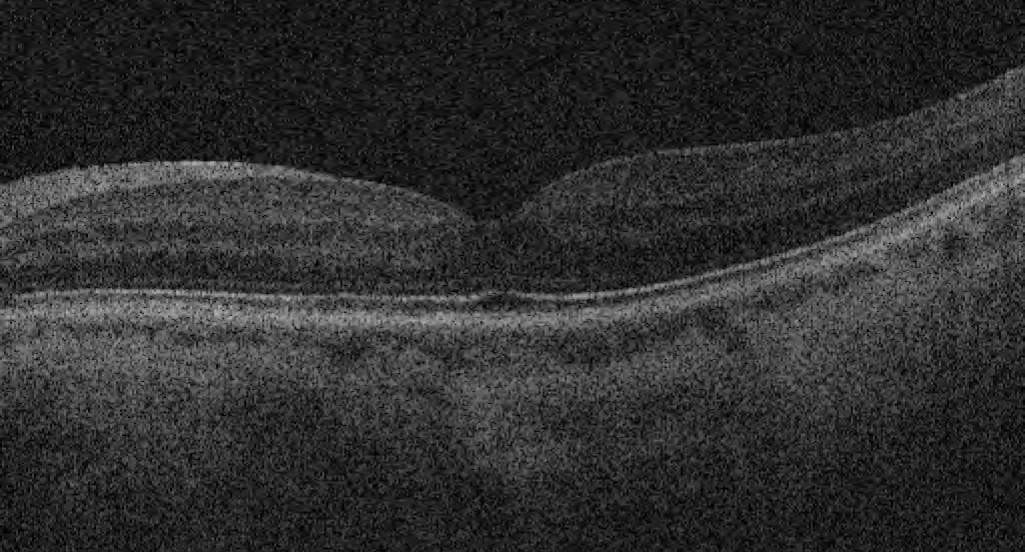
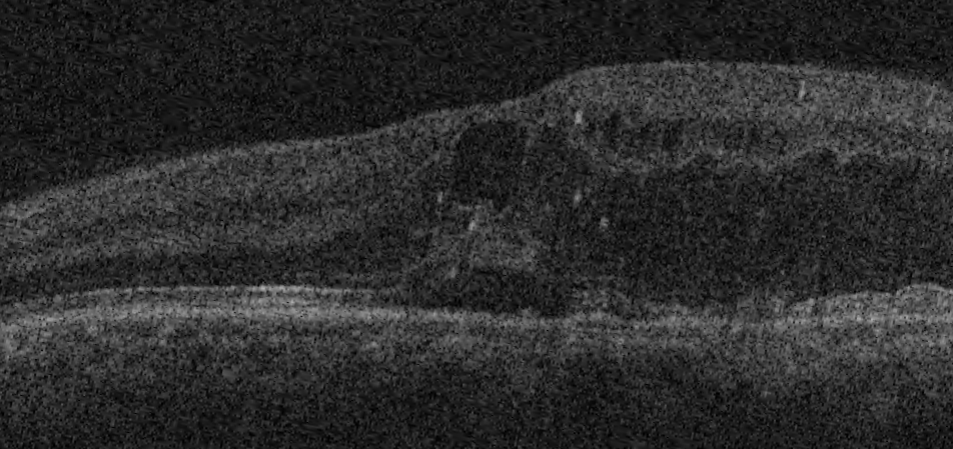
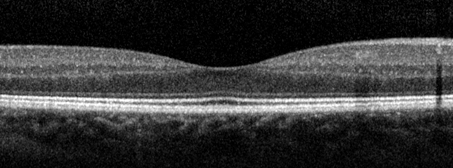
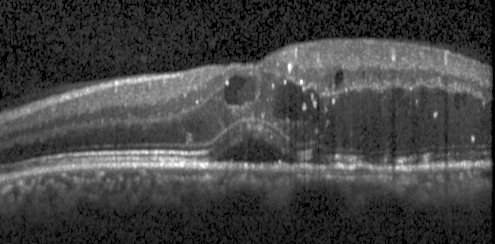
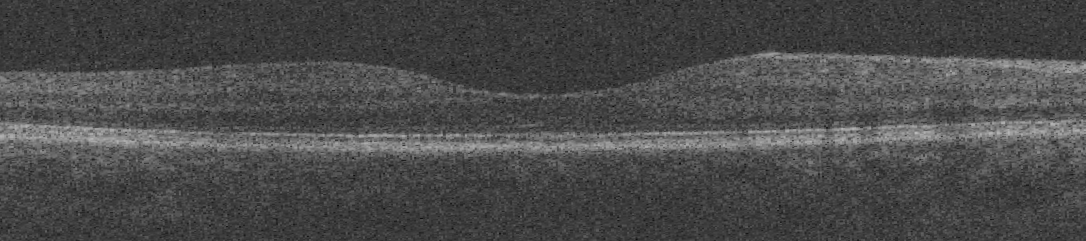
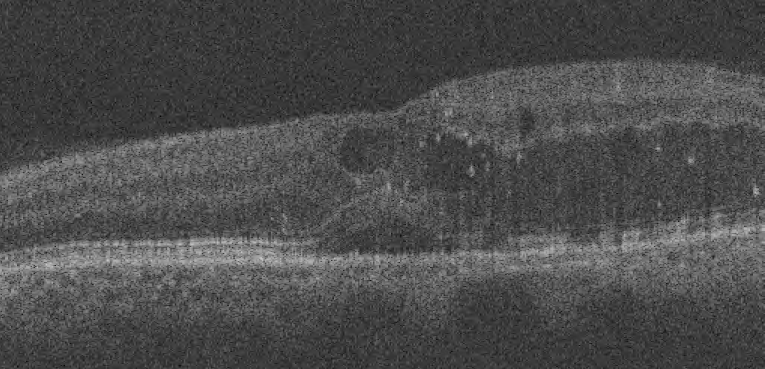
Typical image variability across these three manufacturers for a normal retina and retina with macular edema is shown below.
Top to bottom: Cirrus, Spectralis, Topcon.
 |
 |
 |
 |
 |
 |
|
Normal retina imaged with OCT from the three manufacturers. The three slices come from three different subjects. |
Retina with macular edema imaged with OCT from the three manufacturers. The slices are of the same patient and approximately at the same anatomical position. |